Major Changes Are Coming to E/M Visits in 2021: Will You Be Ready?
Erin Solis, AAFP Manager, Practice and Payment
Significant changes are coming to office/outpatient evaluation and management visit coding and payment, and the AAFP is rolling out resources to help members take full advantage of them. Updates are scheduled to take effect on Jan. 1, 2021 and the Academy is urging members to act now.
In response to advocacy from the AAFP and other organizations, the AMA revised the methodology to document and select CPT levels for office visit E/M services in 2019. CMS will use the updated methodology, meaning its 1995 and 1997 guidelines will no longer apply, and the Academy is advocating for uniform adoption of the changes across all payers.
The changes are intended to increase the amount of time physicians can spend with patients and reduce administrative burden. Physicians will have the option to select the level of code using either total time on the date of service or level of medical decision-making. Further, the definition of total time will expand to include all time personally spent by the physician or qualified health care professional in the care of the patient, both face-to-face and nonface-to-face time on the date of the encounter. In addition, criteria for medical decision-making levels will also be updated. The patient history and physical exam elements will be eliminated as components of office visit E/M code level selection.
Medicare has also created a new Healthcare Common Procedure Coding System code, or G code, for primary care. The new code is intended to represent the visit complexity inherent to E/M services that serve as the continuing focal point for all needed health care services and/or medical care services that are part of ongoing care related to a patient’s single, serious or complex chronic condition. The add-on code will be added to E/M services. Medicare anticipates that all E/M services provided by a primary care physician will qualify for the add-on code.
Though the changes don’t go into effect until 2021, practices should begin preparing now. Here are highlights of key changes being implemented.
History and physical exam codes eliminated (when not appropriate): The patient history and physical exam elements will no longer be components of E/M level code selection. These elements may still be required in relationship to malpractice and quality measures. An understanding of all external documentation guidelines will be necessary before excluding these elements.
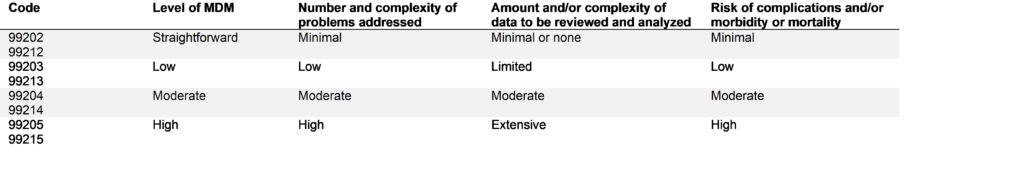
99201 is no longer a valid code: CPT code 99201 will be deleted and will no longer be available as a CPT code selection.
1995/1997 guidelines will be replaced by medical decision making (MDM) or total time: The 1995 and 1997 guidelines will no longer apply. Physicians will have the option to select the level of visit using either total time or medical decision making (MDM). The definition of total time in CPT code selection is expanded to include all time (both face-to-face and non-face-to-face) spent in care of the patient on the day of the encounter. The elements of MDM have been updated. See below for more details on selecting E/M codes by total time or MDM.
- Selecting E/M codes by total time– Total time may be used alone to select the appropriate code level for the office or other outpatient E/M services codes (99202-99205, 99212-99215). Total time is the cumulative amount of time spent in care of the patient on the date of the encounter, inclusive of face-to-face and non-face-to-face time spent by the physician and/or other qualified health care professionals. It includes activities such as review of tests; obtaining and/or reviewing separately obtained history; ordering medications, tests or procedures; documentation of clinical information in the medical record
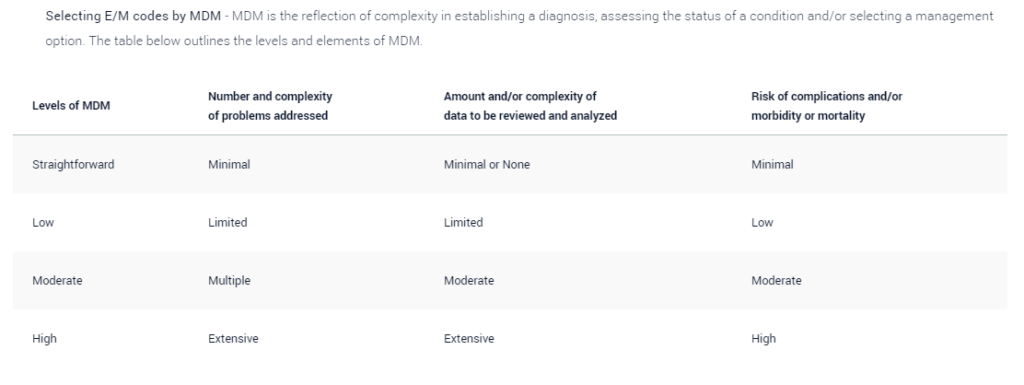
- Selecting E/M codes by MDM – MDM is the reflection of complexity in establishing a diagnosis, assessing the status of a condition and/or selecting a management option. The table below outlines the levels and elements of MDM.
Higher Pay in 2021
Although the transition will take some effort, family physicians should see a payoff on that investment. In addition to the changes in coding, the 2021 Medicare physician fee schedule is slated to include a 13% increase in allowed charges for family medicine. This includes an increase to the relative value units (RVUs) for office/outpatient E/M visits in 2021. Commensurate with that increase, CMS proposes to revalue the following code sets that include, rely upon, or are analogous to office/outpatient E/M visits that impact primary care:
- Transitional Care Management (TCM) Services,
- Maternity Services,
- Cognitive Impairment Assessment and Care Planning, and
- Initial Preventive Physical Examination (IPPE) and Initial and Subsequent Annual Wellness (AWV) Visits.
Get Started with These Resources: 2021 Office Visit Evaluation and Management Documentation Changes:
- A Checklist for Solo and Independent Physicians – This checklist is designed specifically to help small, solo, and independent practices understand steps to take throughout 2020 to ensure readiness in 2021. The AAFP will provide additional resources to help you with the checklist.
- A Checklist for Employed Physicians – This Checklist offers steps employed physicians can take to better understand their employer’s training plan and ensure that their employment contracts are updated appropriately.
- Practice Training Outline – This sample training outline will help your practice implement the updated E/M guidelines. Use it as a guide to ensure you and your staff understand the key concepts and documentation changes.
- Questions to Ask Your Vendors – The updated documentation guidelines will affect multiple aspects of a practice, including your EHR. The AAFP has developed a set of important questions to help you gather key information on your vendor’s plans.
- Questions to Ask Your Payers– Use this resource as a guide for conversations with your payers. Practices will need to understand the impact on their contracts, as well as what training/support the payer plans to offer.
- Template Payer Letter– The AAFP will continue to advocate for uniform adoption of changes across all payers, and you can help by contacting the payers you work with. Use this template to send a letter to private payers to encourage them to adopt the same payment policy changes for E/M codes.
- Talking Points for Employed Physicians – Use this resource to determine if you should have a conversation with your administrator about how the revaluation of codes will impact your pay, or if a contract amendment is appropriate for you.
About the Author
By: Erin Solis, AAFP Manager, Practice and Payment